Geza Ulole
JF-Expert Member
- Oct 31, 2009
- 59,384
- 79,983
- Thread starter
- #281
Geza I have told you again and again that Tz only have hospitals on paper but kwa ground hakuna vitu. When will you stop posting links and tweets and start showing us medical equipment? If we talk of for example protozoology, how will you treat Barbesia if you don't have equipment? What about Theileria?He can respond to ones I mentioned! You komora096 n Teargass tried to mention them n the number of proper county referral hospitals couldn't get to 5! Refer posts #84 n #107! See the hospitals in liked at post #53! They r Mama lucy Kibaki and Nyeri county hospital! The rest r ufisadi aside shoddy job!
Umetoa kichapo heavy hadi Wameanza kulia lia 😂😂😂Only the best? then so many of them in Tanzania as i picked from Zonal to Regional referral hospitals to city and district and town hospitals to health centers! Those r the Public hospitals owned by GoT! stop hating the guy JPM is doing a good job 350 health centers, 94 hospitals around the country for phase I n phase II is coming!
Geza I have told you again and again that Tz only have hospitals on paper but kwa ground hakuna vitu. When will you stop posting links and tweets and start showing us medical equipment? If we talk of for example protozoology, how will you treat Barbesia if you don't have equipment? What about Theileria?
Tunaposema county refferal hospital huaga unaelewa nn?He can respond to ones I mentioned! You komora096 n Teargass tried to mention them n the number of proper county referral hospitals couldn't get to 5! Refer posts #84 n #107! See the hospitals in liked at post #53! They r Mama lucy Kibaki and Nyeri county hospital! The rest r ufisadi aside shoddy job!
Ukwel ni kwamba, vitu kw ground ni different..km hospital ni tweets na maneno ya wana ccm ni sawa..Geza I have told you again and again that Tz only have hospitals on paper but kwa ground hakuna vitu. When will you stop posting links and tweets and start showing us medical equipment? If we talk of for example protozoology, how will you treat Barbesia if you don't have equipment? What about Theileria?
Believe me not to this level!Ukwel ni kwamba, vitu kw ground ni different..km hospital ni tweets na maneno ya wana ccm ni sawa..
Manake mi ninavyojua hospitali ni vifaa, lkn kw geza ulole hospitali kwake ni tweets






Uhuru wa kujieleza huo..tena ana haki ya kuuliza.Tunaposema county refferal hospital huaga unaelewa nn?
Tuanzie hapo kwanza..
Believe me not to this level!
Uhuru wa kujieleza huo..tena ana haki ya kuuliza.
Kituo cha Afya (Health Centre)Hospitali ya Rufaa hii ama Zahanati tu?






Tunaposema county refferal hospital huaga unaelewa nn?
Tuanzie hapo kwanza..
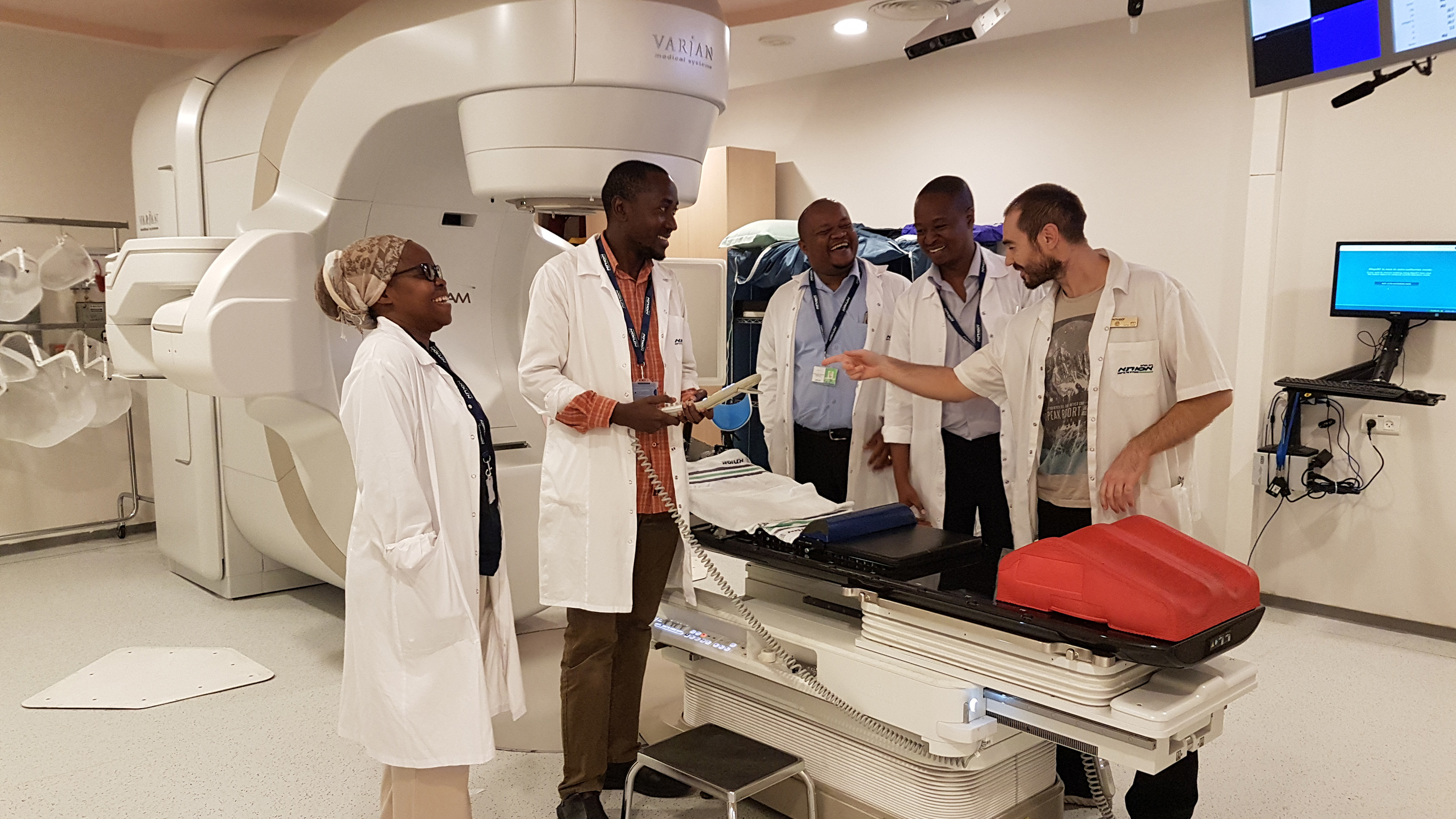
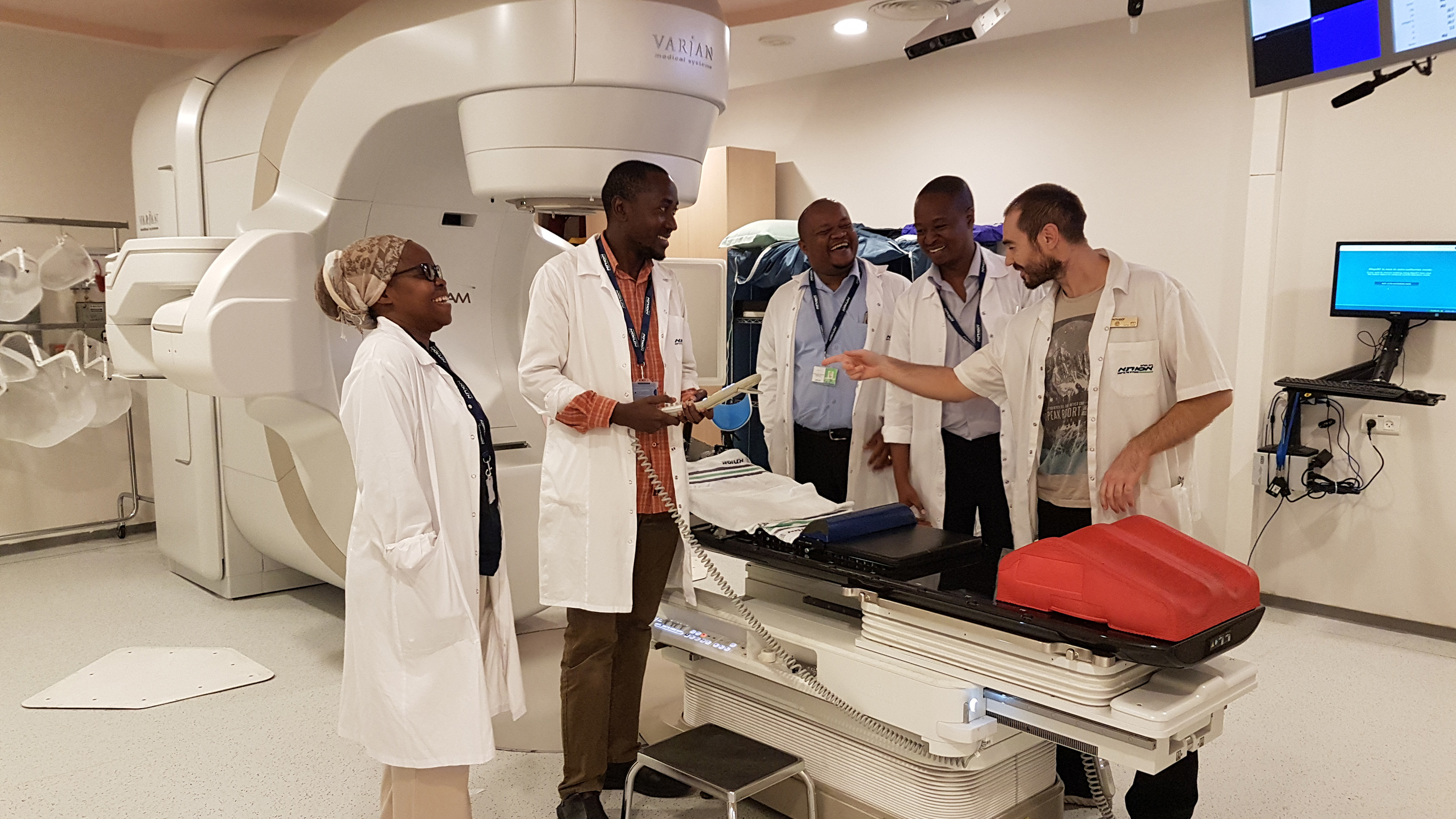
Israel Offers Training in Advanced Radiotherapy to Tanzanian Cancer Care Professionals with IAEA Support
Tanzanian cancer specialists have completed advanced radiotherapy training at leading Israeli cancer centres this month as part of Tanzania’s upgrade of treatment services for common cancers. This leads the way for further opportunities to train African cancer professionals through a new...www.iaea.org
Make Use of Google!Jibu hili swali
Mbna unalikwepa
Heheee!!sasa mbna huaga zinakuumiza na wakati umeenda google ukajua maana ya refferal hospitalMake Use of Google!
Jamaa hata wameshindwa na Uganda alafu wankuja hapa kupiga kelele
View attachment 1258656
Source https://www.sdindicators.org/sites/sdi/files/826660ESW0Ugan090Box379862B00OUO090 .pdf
The report says that 42% of Uganda medics cannot accurately diagnose major diseases. The situation is worse in public health centres offering only outpatient services where half of the providers diagnosed none or only one of five tracer conditions.
An estimated 58% of Uganda's medics got the diagnosis accurate, compared to 72% in Kenya, 57% in Tanzania and 34% in Senegal.
Ugandan public providers managed to correctly diagnose only slightly more than half (56%) of the trace conditions. Only 35% of public health providers could correctly diagnose at least four out of five common conditions (like diahoria with dehydration and malaria with anemia).
"Worryingly, public providers followed only one out of five (20%) of the correction actions needed to manage maternal and neonatal complications,? the report states.
Even when providers correctly diagnose a condition there no guarantee the patient will be treated.
"Indeed the correct treatment was rrecommended in only 36%of the cases, reflecting Weak provider knowledge,? says the service Delivery report whose aim the World Bank said, Is to spur accountability.
"Doctors in Uganda performed at about the Same level as Kenyan nurses on both diagnostic accuracy and the capability to provide full treatment, "it adds.
The SDI initiative is a partnership of the World Bank, the African economic research
Consortium and the African Development Bank to track service delivery performance in sub-Saharan Africa over time.
The preliminary report, launched in November last year was based on surveys of about 400 Health facilities and nearly 2500 health providers Country wide.
The researchers assessed quality in the Health sector using two indicators: adherence Clinical guidelines in five tracer conditions and the management of maternal and newborn complications; and diagnostic accuracy in five tracer conditions.
Three of the tracer conditions were child hood conditions (malaria with anaemia acute)
Diarrhoea with severe dehydration and pneumonia), and two were adult conditions (pulmonary tuberculosis and diabetes mellitus).
The other two conditions included post-partum haemorrhage, the most common cause of material death during birth and neonatal asphyxia, which is the most common cause of neonatal death during birth.
Uganda performed better than Kenya on input indicators and adherence to guidelines. However, Kenya health providers were 20% more likely to get the diagnosis right and were twice as likely to correctly manage maternal and neonatal complications.
Health providers in Senegal and Tanzania performed poorly compared to Uganda and Kenya on diagnostic accuracy, adherence to guidelines and input indicators.
Although almost nine out of 10 (88%) providers were able to correctly diagnose pulmonary tuberculosis, nearly half (47%) did not prescribe the correct treatment required.
Malaria and anaemia were the least likely to be correctly diagnosed and less than one in 10 receiving the correct treatment.
"It is particularly worrying that so few health providers were able to even diagnose potentially deadly conditions such as malaria and diarrhoea," the report says.
Health providers in private health facilities were not consistently better than their counter parts in the public sector .Also, there were large differences across different parts of the country, with health providers in northern Uganda being the worst performers.
Uganda medics (48%) were, however, the best in adhering to clinical guidelines, followed by medics in Kenya (44%), Tanzania (34%) and then Senegal (22%).
Ugandan medics respond
Robinah Karitirimba, the executive director of Uganda national health users /consumers Organisation (UNHCO), disputed the report, saying the study was conducted in the lower health centre 2and 3s where diagnosis is likely to be poor because there a no doctors.
"There is something missing in the report but of course it raises something important about our health care system because most patients go to the lower health centres," she explained.
Kaitiritimba also disputed the allegation that the quality of Ugandan doctors is lower than that of their Kenyan colleagues. She said the only difference is that Kenya has a strong medical associations and the medics are better motivated.
Dr Katumba Ssentongo, the Uganda medical and dental practitioners council registrar, said cases of wrong diagnosis were exaggerated.
"Any practitioner can give wrong diagnosis at certain point .It happens even in Europe, but not to the levels the report put it."
2013 report? How is Kenya situation faring in the last 3 years where strikes r never ending?Jamaa hata wameshindwa na Uganda alafu wankuja hapa kupiga kelele
View attachment 1258656
Source https://www.sdindicators.org/sites/sdi/files/826660ESW0Ugan090Box379862B00OUO090 .pdf
The report says that 42% of Uganda medics cannot accurately diagnose major diseases. The situation is worse in public health centres offering only outpatient services where half of the providers diagnosed none or only one of five tracer conditions.
An estimated 58% of Uganda's medics got the diagnosis accurate, compared to 72% in Kenya, 57% in Tanzania and 34% in Senegal.
Ugandan public providers managed to correctly diagnose only slightly more than half (56%) of the trace conditions. Only 35% of public health providers could correctly diagnose at least four out of five common conditions (like diahoria with dehydration and malaria with anemia).
"Worryingly, public providers followed only one out of five (20%) of the correction actions needed to manage maternal and neonatal complications,? the report states.
Even when providers correctly diagnose a condition there no guarantee the patient will be treated.
"Indeed the correct treatment was rrecommended in only 36%of the cases, reflecting Weak provider knowledge,? says the service Delivery report whose aim the World Bank said, Is to spur accountability.
"Doctors in Uganda performed at about the Same level as Kenyan nurses on both diagnostic accuracy and the capability to provide full treatment, "it adds.
The SDI initiative is a partnership of the World Bank, the African economic research
Consortium and the African Development Bank to track service delivery performance in sub-Saharan Africa over time.
The preliminary report, launched in November last year was based on surveys of about 400 Health facilities and nearly 2500 health providers Country wide.
The researchers assessed quality in the Health sector using two indicators: adherence Clinical guidelines in five tracer conditions and the management of maternal and newborn complications; and diagnostic accuracy in five tracer conditions.
Three of the tracer conditions were child hood conditions (malaria with anaemia acute)
Diarrhoea with severe dehydration and pneumonia), and two were adult conditions (pulmonary tuberculosis and diabetes mellitus).
The other two conditions included post-partum haemorrhage, the most common cause of material death during birth and neonatal asphyxia, which is the most common cause of neonatal death during birth.
Uganda performed better than Kenya on input indicators and adherence to guidelines. However, Kenya health providers were 20% more likely to get the diagnosis right and were twice as likely to correctly manage maternal and neonatal complications.
Health providers in Senegal and Tanzania performed poorly compared to Uganda and Kenya on diagnostic accuracy, adherence to guidelines and input indicators.
Although almost nine out of 10 (88%) providers were able to correctly diagnose pulmonary tuberculosis, nearly half (47%) did not prescribe the correct treatment required.
Malaria and anaemia were the least likely to be correctly diagnosed and less than one in 10 receiving the correct treatment.
"It is particularly worrying that so few health providers were able to even diagnose potentially deadly conditions such as malaria and diarrhoea," the report says.
Health providers in private health facilities were not consistently better than their counter parts in the public sector .Also, there were large differences across different parts of the country, with health providers in northern Uganda being the worst performers.
Uganda medics (48%) were, however, the best in adhering to clinical guidelines, followed by medics in Kenya (44%), Tanzania (34%) and then Senegal (22%).
Ugandan medics respond
Robinah Karitirimba, the executive director of Uganda national health users /consumers Organisation (UNHCO), disputed the report, saying the study was conducted in the lower health centre 2and 3s where diagnosis is likely to be poor because there a no doctors.
"There is something missing in the report but of course it raises something important about our health care system because most patients go to the lower health centres," she explained.
Kaitiritimba also disputed the allegation that the quality of Ugandan doctors is lower than that of their Kenyan colleagues. She said the only difference is that Kenya has a strong medical associations and the medics are better motivated.
Dr Katumba Ssentongo, the Uganda medical and dental practitioners council registrar, said cases of wrong diagnosis were exaggerated.
"Any practitioner can give wrong diagnosis at certain point .It happens even in Europe, but not to the levels the report put it."